Stress-Induced Visceral Adipose Tissue Accumulation
Educational exploration of why chronic stress preferentially increases visceral fat storage.
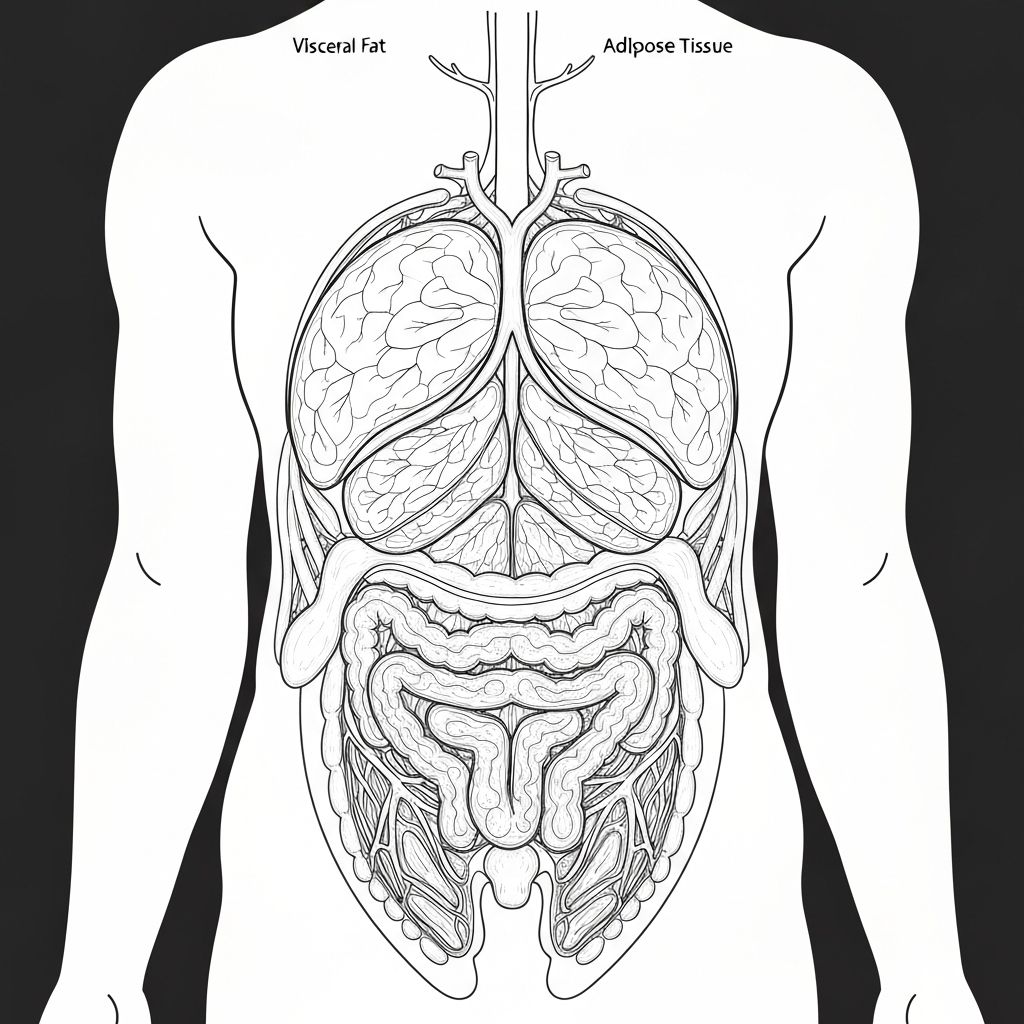
Visceral vs Subcutaneous Adipose Tissue
The body stores fat in two anatomically distinct compartments. Subcutaneous adipose tissue is stored beneath the skin and is distributed throughout the body. Visceral adipose tissue is stored in the peritoneal cavity surrounding abdominal organs—the liver, stomach, intestines, and other organs. These two fat depots differ not only in location but also in metabolic characteristics, hormonal sensitivity, and inflammatory properties. Visceral fat is metabolically more active and inflammatory compared to subcutaneous fat, which has metabolic and health implications.
Chronic glucocorticoid exposure preferentially promotes accumulation in visceral depots over subcutaneous depots.
Glucocorticoid Receptor Distribution
A primary mechanism underlying preferential visceral fat accumulation involves the differential distribution of glucocorticoid receptors across adipose tissue depots. Visceral adipose tissue expresses glucocorticoid receptors at higher density than subcutaneous tissue. Because glucocorticoid effects on adipose tissue metabolism are receptor-mediated, the higher density of receptors in visceral tissue means this compartment is more sensitive to cortisol's metabolic actions. Consequently, when cortisol levels are elevated, visceral adipose tissue receives a stronger metabolic "signal" favouring fat storage compared to subcutaneous tissue.
Cortisol's Metabolic Actions in Adipose Tissue
Cortisol acts within adipose tissue to promote fat storage through multiple mechanisms. First, cortisol increases the expression of lipoprotein lipase (LPL), the enzyme responsible for hydrolysing triglycerides in circulating lipoproteins (chylomicrons and VLDL) and releasing free fatty acids that can be taken up and stored in adipose tissue. Second, cortisol promotes lipogenesis—the synthesis of fatty acids from glucose and other substrates. Third, cortisol reduces lipolysis (fat breakdown), thereby promoting net fat accumulation. These effects occur in both visceral and subcutaneous tissue but are particularly pronounced in visceral tissue due to its higher glucocorticoid receptor density.
Portal Blood Circulation
Visceral adipose tissue drains directly into the portal blood circulation, which delivers nutrients and metabolic by-products directly to the liver. Subcutaneous adipose tissue, by contrast, drains into systemic circulation. This anatomical difference means that free fatty acids released from visceral lipolysis directly reach the liver, potentially disrupting hepatic metabolism and contributing to fatty liver disease under conditions of chronic visceral fat mobilisation. The metabolic consequences of visceral fat redistribution differ from those of equivalent subcutaneous fat accumulation, contributing to distinct health implications.
The "Portal Hypothesis"
The portal hypothesis proposes that visceral fat's unique metabolic consequences—including impaired glucose tolerance and hepatic lipid accumulation—result from the direct delivery of metabolic by-products to the liver. Chronic stress with elevated cortisol may preferentially expand visceral stores due to higher receptor density, and these expanded stores may have greater metabolic impact on whole-body glucose regulation and lipid metabolism compared to subcutaneous expansion of equivalent magnitude.
Inflammatory Characteristics
Visceral adipose tissue exhibits greater pro-inflammatory characteristics than subcutaneous tissue, producing higher amounts of inflammatory cytokines such as TNF-α, IL-6, and IL-1β. Chronic cortisol elevation can paradoxically enhance the inflammatory state of visceral adipose tissue despite cortisol's general immunosuppressive properties, creating a state of "metabolic inflammation." This inflammatory state may contribute to insulin resistance and metabolic dysfunction associated with visceral obesity.
Genetic and Developmental Factors
Individual differences in visceral vs subcutaneous fat distribution are partially determined by genetic factors. Some individuals are genetically predisposed to store fat preferentially in visceral depots, whilst others tend toward subcutaneous storage. Early-life nutrition and developmental factors also influence adipose tissue distribution patterns. These biological predispositions interact with stress exposure, creating substantial individual variability in how chronic stress influences fat distribution patterns.
Research Evidence
Animal and human studies consistently document preferential visceral fat accumulation during chronic stress or glucocorticoid exposure. Imaging studies (CT, MRI) quantifying visceral and subcutaneous adipose tissue volumes in chronically stressed populations show disproportionate visceral expansion. Cell culture and animal model studies demonstrate enhanced sensitivity of visceral adipocytes to glucocorticoid-stimulated fat storage. This convergent evidence supports the concept of stress-induced preferential visceral adiposity.
Clinical and Metabolic Significance
The preferential accumulation of visceral adipose tissue under chronic stress has important metabolic implications. Visceral obesity shows stronger associations with insulin resistance, dyslipidaemia, and metabolic syndrome compared to subcutaneous obesity of equivalent magnitude. Understanding that chronic stress may preferentially drive visceral accumulation helps explain why chronically stressed populations sometimes show metabolic dysfunction disproportionate to total body weight change.
Important Note: This information is educational only. It describes general physiological mechanisms but does not constitute medical advice. Individual fat distribution patterns respond diversely to stress. Consult qualified healthcare professionals for concerns about your health or metabolism.